"I could not be more pleased with my outcome"
- Bill M
What does the prostate do, anyway?
The prostate is a gland that sits just under the urinary bladder. It makes fluid that helps protect sperm. Your sperm move up from your testes into the pelvis where they mix with some fluid from the seminal vesicles as well as the fluid from the prostate. All three components are called semen.
What is a normal size for the prostate?
A normal prostate is the size of a walnut.
The size of the prostate is often referred to in volume (how many cc's) or mass (how many grams)
Normally, the prostate is no larger than 24g; it increases with age, and men often remain free of symptoms until it is larger than 38g
TURP can be performed on the prostate as long as it is smaller than 90g
Once it is larger than 90g, prostatectomy is the only viable surgical option.
The size of the prostate is often referred to in volume (how many cc's) or mass (how many grams)
Normally, the prostate is no larger than 24g; it increases with age, and men often remain free of symptoms until it is larger than 38g
TURP can be performed on the prostate as long as it is smaller than 90g
Once it is larger than 90g, prostatectomy is the only viable surgical option.
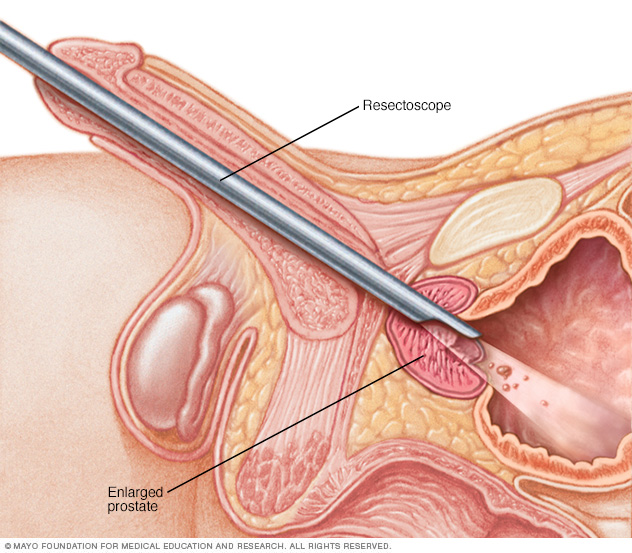
What is a TURP?
TURP stands for TransUrethral Resection of the Prostate. During a TURP a cutting device is advanced up your urethra and used to shave the prostate where it bulges in on the urethra.
I heard that lasers or steam can be used to shrink the prostate rather than a TURP
There are a variety of tools that can be placed into your urethra and used to destroy the tissue of the prostate. With TURP that tissue is carved away. These others destroy the tissue without removing it and include laser, RFA and steam (to destroy by burning) and cryoablation (to destroy by freezing)
What are the chances PAE will work for me?
The team led by Dr. Pisco in Portugal recently published the midterm and longterm results of PAE
Here is the abstract of that article. Bottom line, at 6 years after the procedure 76% of men had benefit without complication.
Abstract
Purpose: To confirm that prostatic artery embolization (PAE) has a positive medium- and long-term effect in symptomatic benign prostatic hyperplasia (BPH).
Materials and Methods: Between March 2009 and October 2014, 630 consecutive patients with BPH and moderate-to-severe lower urinary tract symptoms refractory to medical therapy for at least 6 months or who refused any medical therapy underwent PAE. Outcome parameters were evaluated at baseline; 1, 3, and 6 months; every 6 months between 1 and 3 years; and yearly thereafter up to 6.5 years.
Results: Mean patient age was 65.1 years ± 8.0 (range, 40–89 y). There were 12 (1.9%) technical failures. Bilateral PAE was performed in 572 (92.6%) patients and unilateral PAE was performed in 46 (7.4%) patients. The cumulative clinical success rates at medium- and long-term follow-up were 81.9% (95% confidence interval [CI], 78.3%–84.9%) and 76.3% (95% CI, 68.6%–82.4%). There was a statistically significant (P < .0001) change from baseline to last observed value in all clinical parameters: International Prostate Symptom Score (IPSS), quality-of-life (QOL), prostate volume, prostate-specific antigen, urinary maximal flow rate, postvoid residual, and International Index of Erectile Function. There were 2 major complications without sequelae.
Conclusions: PAE had a positive effect on IPSS, QOL, and all objective outcomes in symptomatic BPH. The medium- (1–3 y) and long-term (> 3–6.5 y) clinical success rates were 81.9% and 76.3%, with no urinary incontinence or sexual dysfunction reported.
Here is the abstract of that article. Bottom line, at 6 years after the procedure 76% of men had benefit without complication.
Abstract
Purpose: To confirm that prostatic artery embolization (PAE) has a positive medium- and long-term effect in symptomatic benign prostatic hyperplasia (BPH).
Materials and Methods: Between March 2009 and October 2014, 630 consecutive patients with BPH and moderate-to-severe lower urinary tract symptoms refractory to medical therapy for at least 6 months or who refused any medical therapy underwent PAE. Outcome parameters were evaluated at baseline; 1, 3, and 6 months; every 6 months between 1 and 3 years; and yearly thereafter up to 6.5 years.
Results: Mean patient age was 65.1 years ± 8.0 (range, 40–89 y). There were 12 (1.9%) technical failures. Bilateral PAE was performed in 572 (92.6%) patients and unilateral PAE was performed in 46 (7.4%) patients. The cumulative clinical success rates at medium- and long-term follow-up were 81.9% (95% confidence interval [CI], 78.3%–84.9%) and 76.3% (95% CI, 68.6%–82.4%). There was a statistically significant (P < .0001) change from baseline to last observed value in all clinical parameters: International Prostate Symptom Score (IPSS), quality-of-life (QOL), prostate volume, prostate-specific antigen, urinary maximal flow rate, postvoid residual, and International Index of Erectile Function. There were 2 major complications without sequelae.
Conclusions: PAE had a positive effect on IPSS, QOL, and all objective outcomes in symptomatic BPH. The medium- (1–3 y) and long-term (> 3–6.5 y) clinical success rates were 81.9% and 76.3%, with no urinary incontinence or sexual dysfunction reported.